3 Key Concepts for Code-Compliant Outpatient Healthcare Facility Design
By Dave Curfman | Feb 01, 2022

Key Takeaways
- Clinic-outpatient and ambulatory health care facilities are the two code-defined categories of outpatient healthcare facilities. Designing them, however, is more than an either-or process.
- An outpatient facility’s specific medical functions directly influence the intensity of MEP design requirements.
- Giving each space the correct name is vital for code compliance and successful accreditation surveys.
Anyone who’s been involved in designing, constructing, or operating a healthcare facility knows that these are heavily code-driven facilities. A host of governing bodies provides rules and regulations specifying everything from room size to acceptable finishes to number of air changes. Questions about code requirements can provoke intense conversations among project team members.
Outpatient facilities present a unique challenge to the design team and the owner’s vision. While hospitals are among the most complex buildings to design, but the code path is reasonably clear. Outpatient facilities, on the other hand, tend to live in more of a gray area when it comes to alignment between the intended space functions and the applicable codes and standards.
From a code standpoint, outpatient facilities are divided into two basic categories: clinic-outpatient and ambulatory health care facilities. But rarely is the process as simple as identifying one of these two building types and proceeding uninhibited with design. More often, it involves an extensive back-and-forth between the design team and the healthcare organization to identify key project requirements, then aligning the design to match. Getting this right is critical for accreditation, functionality, and patient safety.
This article outlines three key points related to outpatient healthcare facility design: the defining characteristics of each facility type, how the design requirements vary in intensity depending on the medical functions, and why it’s vital to give the correct name to each space in the building.
1. Clinic-Outpatient and Ambulatory Health Care Facilities: What’s the Difference?
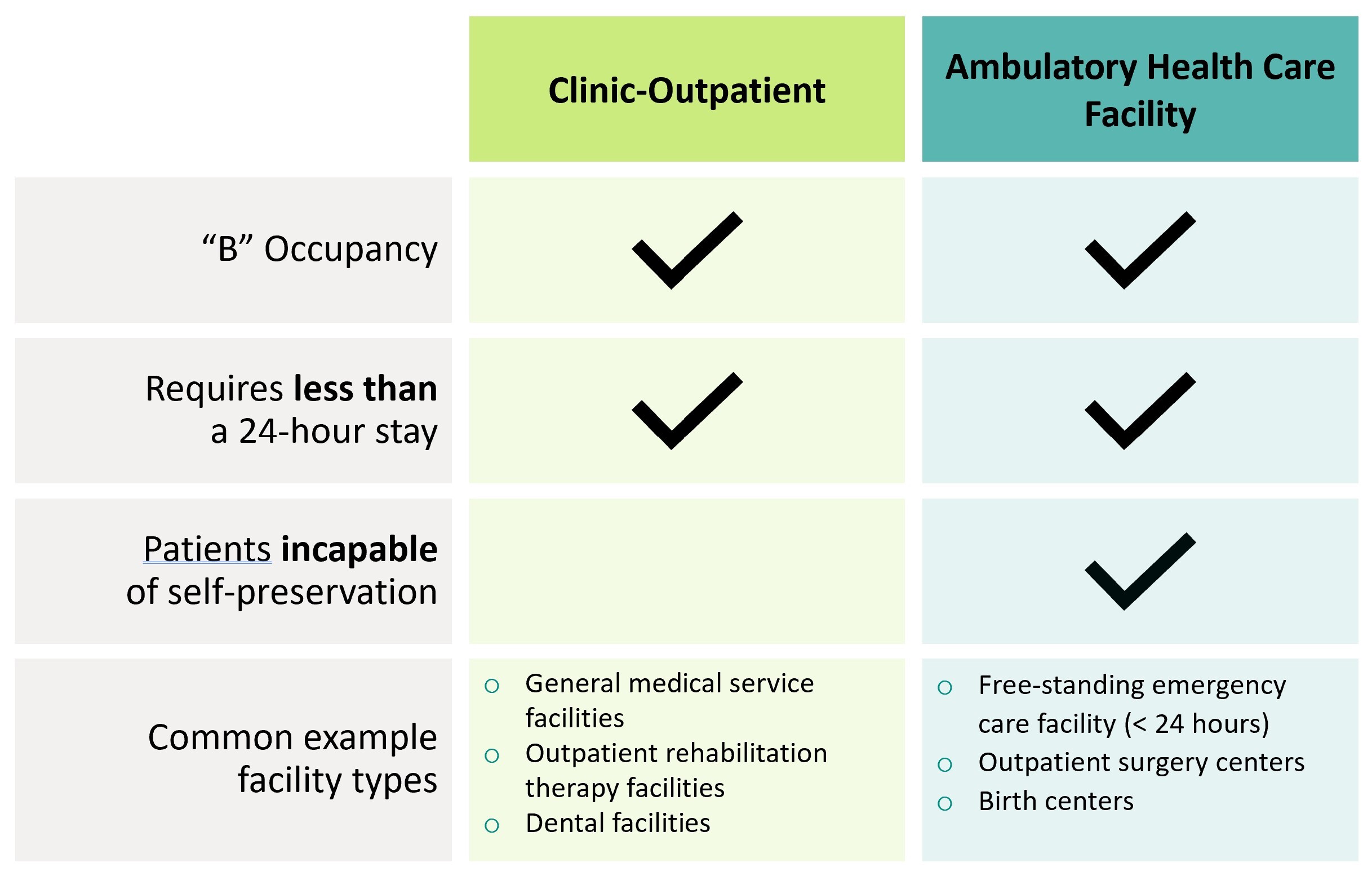
The terms “Clinic-Outpatient” and “Ambulatory Health Care Facility” come to us from the International Building Code 2015. Both are “B” occupancy facilities and, unlike hospitals, require that patients have less than a 24-hour stay.
An important distinction between the two facility types has to do with patients’ capacity for self-preservation. In clinic-outpatient facilities, patients are capable of self-preservation, while in ambulatory healthcare facilities, patients may be incapable of self-preservation. As a result, the MEP system design requirements can be dramatically different, which in turn can impact the project cost and space programming.
2. The Sliding Scale of MEP Design Intensity
Figuring out whether the building is a clinic-outpatient or an ambulatory health care facility guides certain big-picture design requirements. For example, designing an ambulatory health care facility means there are some MEP systems you have to have, such as emergency power. But that doesn’t mean that your clinic-outpatient won’t need a generator – that is also possible.
Neither category is a one-size-fits all. Clinic-outpatient buildings can be as simple as a storefront dentist’s office, while ambulatory health care facilities can be just short of a full-blown hospital, as is often the case with ambulatory surgery centers. In between these two extremes is a wide range of options and, as a result, a wide range of MEP system intensity.
The real key to a proper design lies in the specific requirements driven by the medical services being provided. These requirements tend to play out as more of a sliding scale of intensity (see graphic below), rather than distinct and separate paths. The more intense the medical services, the more intense the supporting MEP.
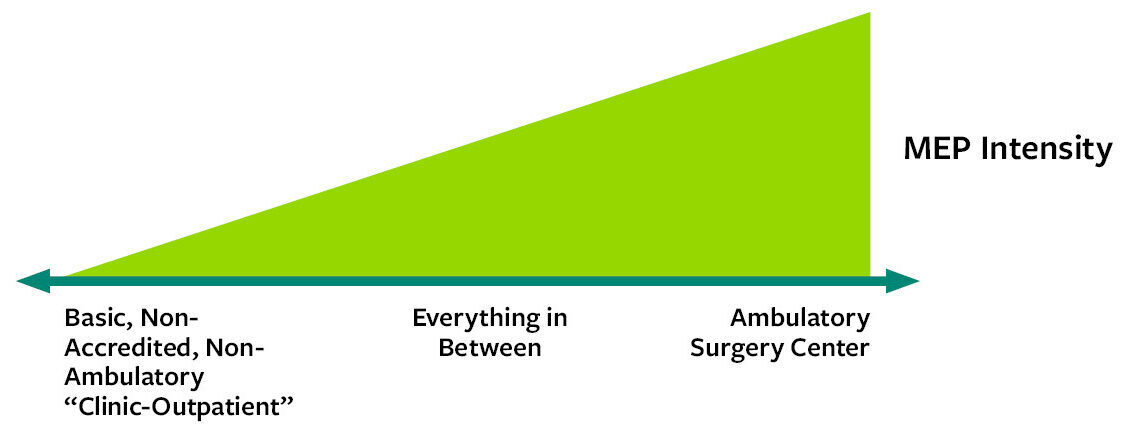
Understanding exactly what services are provided in these buildings can dramatically change what system have to go in them and the associated cost of construction. Some MEP items might be entirely preference in one building, but in another very similar building they become mandatory infrastructure supporting a specific healthcare offering.
A healthcare organization might anticipate that because they want a basic doctor’s office, they can build a basic office building for creature comfort and be done. But as soon as the facility is accredited and billing to Medicare or Medicaid, certain healthcare-specific design requirements likely come into play (e.g., air changes, filtration requirements). It doesn’t take much to trigger additional requirements: The building could have a single space providing a specific healthcare service that triggers additional MEP features for the whole building.
At the outset of a project, it’s critical for the team to identify what specific services the facility will provide. What will they be offering on Day 1? What might they be offering two years down the road? What if the healthcare organization brings on a new doctor to provide a specific type of procedure? The answers to these questions can affect everything from room size to temperature control capabilities to air handler configurations.
3. The Importance of Matching Room Name and Space Function
When someone gives me a floor plan, inevitably what happens is that someone says, “Here are 10 exam rooms.” Easy enough. With only a few basic questions, we can confirm what’s needed for the exam rooms and move forward.
Then we come across a space labeled something like “lab” or “procedure.” Terms like these are trigger words because they have specific meanings in the applicable codes and standards (and can have different meanings from one standard to the next). They cue us to drill down and learn exactly what services caregivers will be providing in these spaces and whether the room name matches the space functions.
“Procedure,” for example, has specific connotations that can really ramp up the MEP requirements. Medical personnel tend to use the word “procedure” for a much wider range of services than what the MEP design codes and standards refer to. If a healthcare provider isn’t actually performing “procedures,” but something more basic, then the room needs a name that will not trigger those code requirements. Often we find that “procedure” rooms should really be “treatment” rooms.
We see something similar with a term like “laboratory.” What kind of laboratory is it? What functions will lab techs be performing? The answers to these questions guide our design decisions, and the room name assigned may inform how an accrediting body will survey that space for compliance.
Specific space functions can impact an entire building’s infrastructure needs. Until the design team knows what the healthcare organization is doing in every corner of the building, they don’t know what it really needs.
Spending time up front learning the details of medical services and understanding the expectations of the caregivers can seem tedious. By doing so, though, the design team exchanges valuable information with the medical team, gains confidence in their product, and stands the best chance of avoiding budgetary and operational issues.